
Prescribing Pilates for Pain Rehabilitation
How would you describe the holistic approach to dealing with pain?
For medical professionals, it means thinking about patients as a whole person and understanding that when someone comes into the office when their hip is hurting them, the problem may be more complicated than just their hip. We may have to factor in a mechanical perspective, we may have to think about how the spine works, how the ankle and foot work, and any asymmetries or movement impairment that may contribute to their pain. That’s a holistic way of thinking about how the body works. It’s what we refer to as the kinetic chain.
We also think about the person as a whole in terms of their social life, their family life, their work, their lifestyle, and how past experiences might contribute in a positive or negative way to the pain they're experiencing.
Why is taking a holistic approach important in treating patients?
Ultimately, by taking this approach, the patient feels cared for. One of my mentors once told me, “Your patient is not going to care how much you know until they know how much you care.” It just fosters that positive relationship in a medical setting.
Of course, when I see someone who sprained their ankle two weeks ago, I may not dive into their personal and medical history as much as I would with someone who is coming in with 10 years of low back pain that has greatly impacted their life in a negative way. I might want to know a lot more about that patient's personal or family history and their medical history.
When you talk about holistic treatment, is that where rehabilitative therapies, like Pilates, come in?
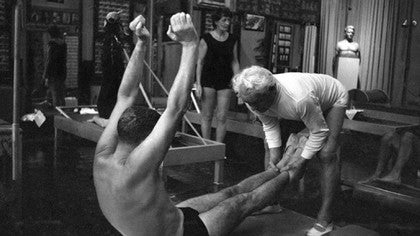
We refer to that as a comprehensive approach. When I recommend physical therapy or Pilates to one of my patients, it is to supplement their treatment program while they are in my care or after they leave my care.How do you work with other professionals such as Pilates teachers in helping rehabilitate your patients or to inform a plan for their care?
I may advise and counsel health care providers based on the feedback I receive. And I think it’s a two-way street; I need to know what my patient is doing outside of their medical care, and how it's going, so I know what am I recommending. If I don’t hear feedback from professionals working with my patients, I assume everything is going well. If I hear my patient is not tolerating a program, I can adjust accordingly. A patient's care doesn't stop because they leave my office.
Did your background in physical therapy lead you to recommend Pilates to your patients?
Probably. As I was learning about core strengthening or core stability programs, Joseph Pilates was commonly referenced in the papers I read. I realized that many rehab principles - whether they are borrowed or modified - are somewhat of a Pilates-based approach. So, I felt comfortable and safe with Pilates and began to recommend it to patients.
Is there an ideal client for whom you recommend Pilates?
I treat a lot of athletes, and I use that term broadly: high school, college, and professional athletes, or someone just trying to stay recreationally active, and everything in between.
Within that scope, there are many people who I can help to relieve low back pain or other issues and to help them to move better, help move them towards their goals. But there are limitations in terms of how long people are in rehabilitation. There may be insurance limitations, their own personal time limitations, or they may be limited by how long they will be in a geographic location. So, Pilates becomes a natural post-rehabilitation exercise program that I recommend.
Often, I will tell my patients they’ve done great with physical therapy, and they now have the tools and a good foundation. They’re doing better, and here’s something that can take them to the next level. That’s a very common situation where I would recommend Pilates.
There also are times where a client has not responded as I would have hoped to traditional therapy, and so based on their condition and my further evaluation, then Pilates may be a safe alternative to consider.
How do you help patients understand what is possible when dealing with pain?
I use a variety of different tools to help people to realize that they can move with less pain or without pain interfering with their movements or their function or their quality of life. Sometimes, that is a medication, such as an injection, that might help them be more active. Or, I might work with them physically in the office, and show them how to posture differently. If they engage certain muscles before they move, they can perform the same movement without pain. That can be really powerful to a patient.
If you think of someone with shoulder pain, and you adjust or assist their scapula so they can do the same movement without pain, you show them there is a possible solution. They have hope. And I think hopelessness or despair is in line with chronic pain and disability. Hope accomplishes the exact opposite.
Is overcoming pain a realistic goal for someone living with chronic pain?
I've never really agreed with the traditional model or concept of pain management. You manage a lot of things in your life. Relationships you manage. You manage your finances because you want to maintain them and help them to grow. So, I don't know if you really want to be managing pain. There are, of course, conditions that are chronic and do not really have a solution. And they do need some sort of management plan.
There’s an old rehabilitation principle that as you help people to become more functional and you help them to accomplish more, reach their goals, especially functional-oriented goals, pain typically and eventually declines to some extent. We need to help people to stop focusing on what their pain feels like and how it limits them. We need to help them shift their focus to what they can accomplish despite their pain.
The pain may not completely resolve, but typically it declines as we're able to do more and as we're able to achieve goals. And I think if we're able to achieve goals, we’re a little bit happier with our day. Happiness and laughter are great treatments for pain. So, I try to just get that shift from focusing on what they can't do to what can they do.
With pain and the current opioid crisis at the forefront of our national conversation, what do you see as the role of professionals, like Pilates teachers, in working with people experiencing pain?
The opioid epidemic just highlights the facts we already know: musculoskeletal conditions like back and neck pain and osteoarthritis are some of the most disabling conditions worldwide. And there obviously were too many patients dependent on a narcotic or opioid medication to manage their pain and keep functioning.
We need to be more creative, more holistic, more comprehensive in putting together plans that help people to better cope with these conditions without the need for potent medications with risks or for routine uses of injections or for surgical treatment.
We should all - not just physicians and health care practitioners, but anyone who can add to the quality of life - be looking to improve the quality of movement for people, the maintenance of movement, and towards prevention of things like falls. We should all be more creative and more collaborative to avoid another coming of an opioid epidemic as we try to emerge from the one we are currently experiencing.
Comments
No comments yet. Be the first!










You need to be a subscriber to post a comment.
Please Log In or Create an Account to start your free trial.